Nursing ed reimagined: Fostering unity, igniting passion, and simulating life
Dr Miriam James-Scotter, a practising primary health care (PHC) nurse and experienced adult literacy teacher, brings an authentic pedagogical approach to the School of Nursing. Her student-centred teaching methods are designed to help students understand their place within the nursing profession and develop the practical skills required in today’s environment. Her methods promote an inclusive learning environment by emphasising relational learning and authentic assessment for learning.

Miriam challenges the conventional mindset that nursing practice ought to only begin in a hospital setting. She emphasises the importance of primary health care (PHC) and strives to change deeply embedded belief systems by igniting passion in her students through connection, community-building, and engagement in tactile, life-like scenarios.
The low-tech method effectively counters the increasing lack of physical engagement in learning. The ungraded, self-guided activities resemble authentic and safe interactive oral assessments.
Teaching methods
Miriam focuses on cultivating relationships between students and subject through simulation of life-like situations and small group work. She also uses scaffolded assessment for learning, which involves no grading but relies on intrinsic student motivation to learn and succeed.
Her contribution to the undergraduate nursing program includes course design, coordination, and teaching of several courses. She also builds connections with communities and PHC centres outside of the University to arrange new placement opportunities for her students.
Miriam has introduced learning materials and assessments that align with both the learning outcomes (LOs) and existing nursing standards.
LO 1: To be able to discuss the application of key theoretical concepts, models and documents underpinning the New Zealand Primary Healthcare System incl. principles of Primary healthcare, Te Tiriti o Waitangi, He Korowai Organa, NZ Health Strategy, Ottawa Charter, Dec/oration of Astana.
LO 2: To be able to identify and compare key features of common New Zealand primary healthcare nursing roles and settings incl. interprofessional team models.
LO 3: To gain on understanding of New Zealand primary and secondary prevention strategies / initiatives relevant to New Zealand PHC nursing, including being able to collaborate and refer to community agencies.
LO 4: To be able to provide evidence-based health education and promotion relating to healthy lifestyles.
LO 5: To develop an understanding of the risk factors, pathophysiology, assessment treatment and education relating to a range of common community presentations for PHC nurses within a range of settings.
LO 6: To be able to critically apply models and concepts related to long-term conditions and consider the role of the PHC nurse in this context.
LO 7: To develop the ability to critically analyse and apply health literacy concepts to improve health promotion strategies.
LO 8: To apply clinical assessment and reasoning skills to the triage and management of common acute community presentations.
Figure 1 – Learning outcomes created to align with the Primary Healthcare Nursing Standards of Practice in NZ.
Scenario-based activities
Miriam has developed three hands-on, interactive learning activities for her 3rd year students. Each activity is carefully designed to provide a tactile experience and establish a personal connection.
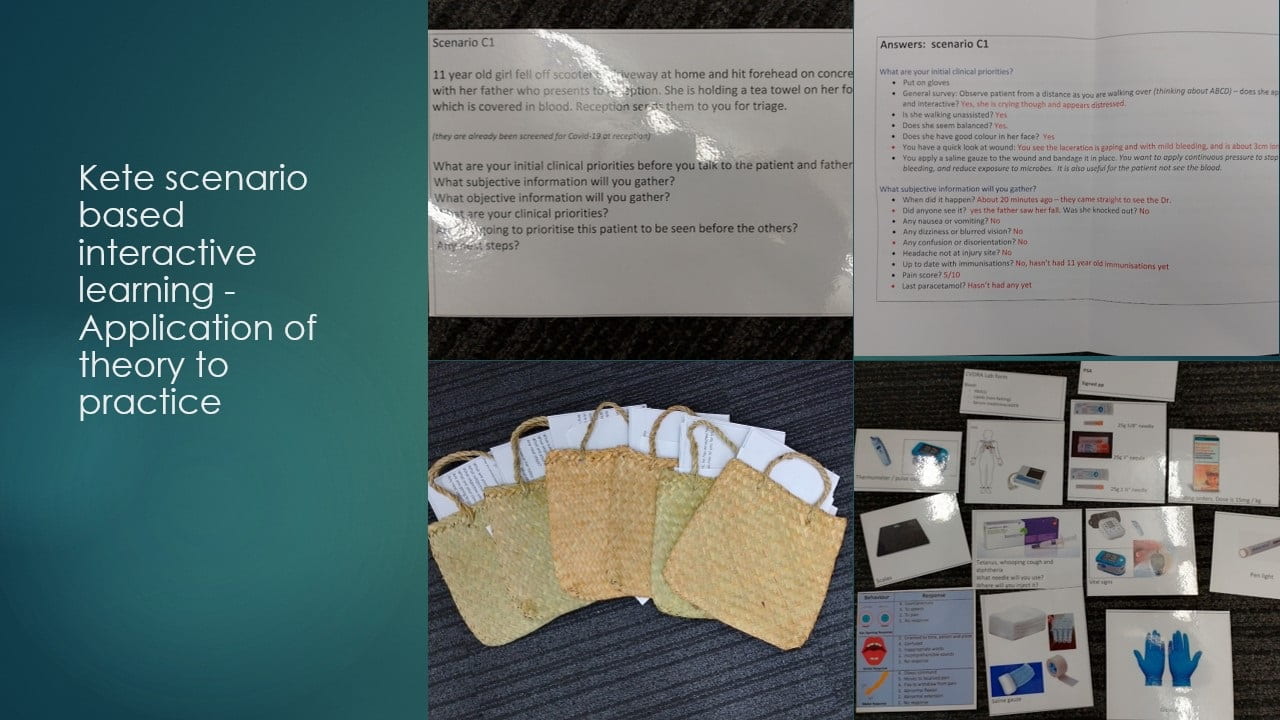
1. PHC Kete scenarios
A group-based activity where students work through real-life scenarios. This activity is part of the Clinical Skills Placement Preparation Day and is designed to be self-directed and student-centred. Students work in groups of three, with two performing the nursing tasks and one holding the answers, clinical assessment results, and prompts. The activity is designed like a game of cards, adding an element of fun to the learning process.
“The activities were great for cementing nursing knowledge for holistic care.”
“The scenarios were a good way to actively try to triage a clients with the help of peers.”
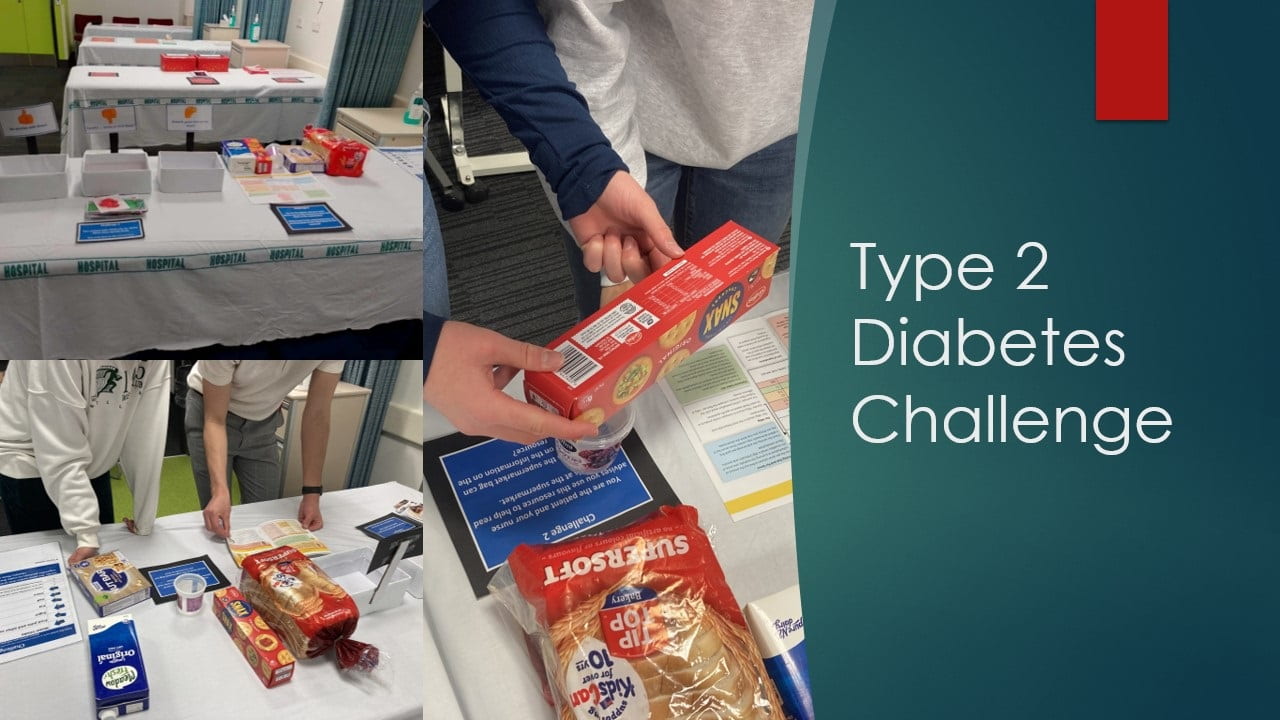
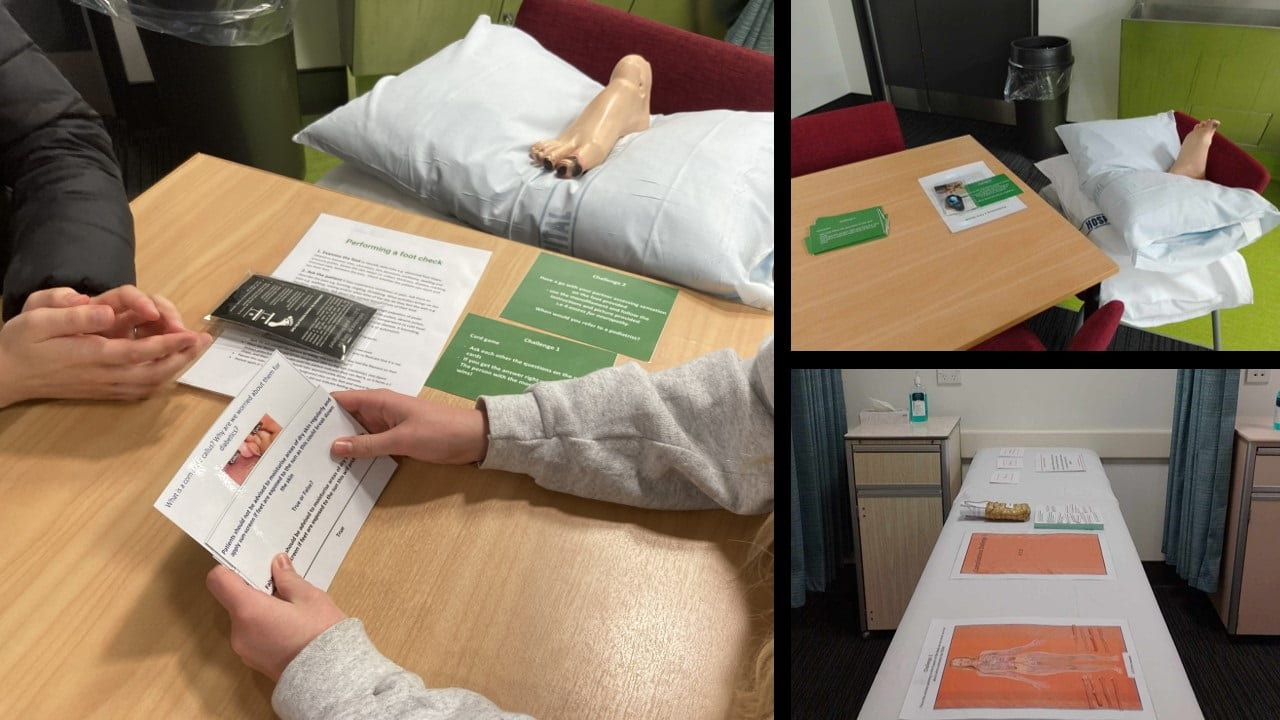
2. Type 2 diabetes challenge
A station-based activity where students apply their knowledge to problem-solving tasks. This activity was designed for 3rd year or pre-registration student nurses. Five stations were created, loosely based on the Annual Diabetic Review, typically conducted in the community by nurses. The activity covers topics relating to management of blood sugars, dietary advice, conducting foot checks, screening for complications and medication management.
Figures 3, 4, 5: Type 2 Diabetes challenge activity kit.
“Diabetes challenge was wonderful, it was a wide variety of activities and sparked a lot of discussion.”
3. PHC Urgent Care Simulation
This role-play is part of NURSING 302: Professional Nursing Practice. It involves actor-patients and a practitioner on the side to direct the nursing activities and answer student questions. It is designed to create a safe and supportive learning environment.
Figures 6, 7, 8: The learning activity simulating nurses’ work at an urgent care clinic.
Learning through real-life placement
A significant change to the programme has been the introduction of a three-week primary healthcare placement in the third year, as part of NURSING 301: Community Health and Wellbeing. This placement allows students to reflect on their experiences and understand the community within which the nursing profession operates.
Summary and reflection
Challenges
Despite the positive feedback, Miriam acknowledges the challenges such as the unsuitability of traditional lecture theatres for her hands-on, practical activities, maintaining her handcrafted teaching materials from wear and tear, needing to regularly update materials, and dissipating student fear. She addresses the latter by creating a safe and supportive learning environment, scaffolding the learning activities, and introducing ungraded assignments.
Impact and student feedback
The initiatives have been well-received by students, with a small increase in new students registering to become nurses for primary healthcare.
Looking ahead
Miriam hopes to work more closely with faculty and clinical partners, review learning outcomes, and introduce more community-based interprofessional simulations.